Uveitis Guide: Types, Symptoms, Causes, and Treatments
Uveitis is a serious eye condition characterized by inflammation of the uvea, the middle layer of tissue in your eye. There are four types of uveitis, distinguished by the part of the uvea they affect.
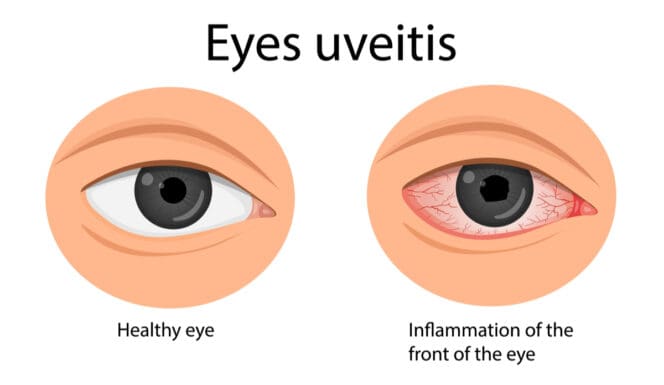
Symptoms include eye pain, redness and loss of vision.
Left untreated, uveitis can lead to serious complications, including glaucoma, retinal detachment and permanent vision loss. Treatment usually involves long-term steroid use which must be carefully controlled to prevent further complications.
Depending on how well the uveitis responds to the steroids, you may need additional treatments to get the condition under control.
Types of Uveitis
There are four types of uveitis: anterior, intermediate, posterior and panuveitis.
- Anterior uveitis (also called iritis) affects the front section of the uvea, including, the tissue between the iris and the cornea, the iris itself, and the ciliary body. This type is usually the easiest to treat.
- Intermediate uveitis affects the middle of the uvea, including the retina, the blood vessels behind the lens and the vitreous (the transparent, gel-like substance in the center of the eye).
- Posterior uveitis affects the back of the uvea, including the retina or the choroid (the tissues that make up the wall in the back of the eye. This type is difficult to treat and is most likely to cause severe complications.
- Panuveitis affects all three layers of the uvea at once. This is the rarest type of uveitis.
Symptoms
Symptoms of uveitis include:
- Eye redness
- Eye pain
- Sensitivity to light
- Blurry vision
- Dark, floating specks (called floaters) passing through your field of vision
- Loss of vision
Symptoms usually come on suddenly, but they can develop gradually in some cases. Sudden usually worsen quickly. Symptoms can appear in just one eye or in both at the same time.
In rare cases, uveitis will present with no symptoms. When this happens, it will usually be found during a routine eye exam.
Causes
Medical researchers do not know the exact causes of uveitis, and few common links have been observed among patients with this condition. Some factors have been linked to a higher risk of developing uveitis, including:
- Eye injury
- Recent eye surgery
- Autoimmune diseases, such as lupus, psoriasis, and sarcoidosis
- Infections like syphilis, shingles or toxoplamosis
Despite the lack of clarity of causation, some diseases and infections are more strongly associated with one type of uveitis. For example, around one-third of people with intermediate uveitis also have sarcoidosis or multiple sclerosis.
Risk Factors
In addition to the infections and disease ties, researchers have built personas of those people more likely to develop uveitis. They include:
- People between the ages of 40 and 60
- People with existing eye conditions
- Women
- Smokers
Experts do not know why these groups are more vulnerable than others to develop uveitis. Many researchers believe that it is because these people are more likely to have higher levels of inflammation in their bodies.
Further research on the causes of uveitis will help to determine the real reason for this difference and identify other groups of people who may be at risk.
Diagnosis
Diagnosing uveitis often involves several steps.
First, your eye doctor will examine your eye using a small handheld light. This is done to get a better look at any redness in your eye and see how your pupil responds to light. Abnormal pupillary responses are a sign of anterior uveitis, the most common of this condition.
To confirm the diagnosis or examine you for other types of uveitis, your eye doctor may also perform some combination of the following:
- A slit-lamp dilated eye exam
- A fundoscopic exam (an examination of the back of the eye)
- A tonometry (ocular pressure) test
- X-rays of the retina
- Testing of vitreous fluid (the fluid inside the center of your eye)
- CT or MRI scans
- Angiography testing of the blood vessels in your eye
Because uveitis is such a rare condition, your eye doctor may ask you some questions about your overall medical history. Your doctor also may recommend getting tested for the types of infections known to cause uveitis. This will help you discover any underlying health conditions you might have and allow you to treat those conditions alongside your uveitis.
Treatment
Doctors treat uveitis with regular doses of steroids, which calm the inflammation, reduce the severity of symptoms and stop the disease from progressing. They deliver steroids in one of a few forms:
- Eye drops
- Injections
- Implants
If steroid treatments do not produce the desired results, your eye doctor may prescribe one or more additional treatments: oral steroids, mydriatic eyedrops or courses of antivirals, antibiotics and antifungals, immunosuppressants or a vitrectomy procedure.
Oral Steroid Medications
Patients can also take steroids can in pill form. Oral steroids are usually much stronger than steroids delivered through other means. As a result, they are also more likely to cause complications during your treatment.
They are only used in rare cases when other treatments have not worked or when uveitis is present at the back of the eye.
Mydriatic Eyedrops
Mydriatic eyedrops treat anterior uveitis by inducing eye dilation. This reduces the pressure in your eye, makes your uveitis less painful and reduces your risk of developing glaucoma as a complication.
However, these drops also make it difficult to see clearly, so they may not be an appropriate treatment for all patients with anterior uveitis.
Antivirals, Antibiotics and Antifungals
Sometimes uveitis does not respond well to treatment until the infection that caused the inflammation has been treated. In these cases, antibiotics, antifungals, or antivirals may be prescribed to help that infection clear up.
Once the infection is under control, the uveitis may clear up on its own or respond better to conventional treatment.
These treatments cannot be administered without first identifying the initial infection, which may be difficult to do. Some cases of uveitis also occur spontaneously without any underlying infection and will not respond to this treatment.
Immunosuppressants
If your uveitis does not improve using first-line treatments or you experience complications from steroid use, your eye doctor may prescribe a course of immunosuppressant medication. The medications lower the effectiveness of your immune system and may calm your uveitis symptoms.
However, immunosuppressants affect your entire body. They make you more susceptible to illness and may make common infections like the flu much worse.
They may also cause unpleasant side effects like headaches, high blood pressure, hair loss, and more. As a result, they should only be used as a last resort.
Vitrectomy
If your uveitis is very severe or caused by a certain type of infection, your eye doctor may recommend that you undergo a type of surgery called a vitrectomy. This procedure uses a long needle to extract the vitreous fluid in the middle of your eye and replace it with a bubble of air or gas. Your eye will naturally refill itself with vitreous fluid over time.
Some mild cases of uveitis go away on their own with no medical treatment. However, it is impossible to predict whether this will happen in your case. If you have uveitis, you must follow the course of treatment your eye doctor recommends to ensure that your condition does not get worse.
Side Effects and Complications
Uveitis is a serious disease. Left untreated, it can lead to:
- Retinal swelling or scarring
- Retinal detachment
- Glaucoma
- Cataracts
- Vision loss
Getting treatment for uveitis can also lead to some serious side effects. Prolonged steroid use can cause a variety of illnesses, including:
- Cataract
- Glaucoma
- Cushing’s syndrome
- Stomach ulcers
- Diabetes
- Heart disease
- Edema (fluid retention and swelling)
These potential side effects do not mean that treatment is not viable or worth pursuing. However, you will need to see your eye doctor and family doctor regularly to monitor your condition and look for early signs of any of these problems.
Prevention
Because eye doctors do not know the cause of uveitis, they struggle to identify effective prevention strategies. However, the following actions may help to lower your risk of developing this disease.
- Seek treatment for any autoimmune diseases you have. Untreated autoimmune diseases generate high levels of inflammation. This may trigger inflammatory diseases like uveitis.
- Eat a balanced diet. Consuming a wide variety of foods provides your body with all the vitamins and minerals it needs for good eye health.
- Exercise. Regular exercise lowers inflammation levels in your body and reduces stress, both of which can reduce your risk of uveitis.
- Stop smoking. Smoking leads to increased inflammation in your body and has been specifically linked to a higher risk of developing uveitis.
- Take a multivitamin. Supplementing your diet with a multivitamin tops up your body’s supply of essential nutrients and antioxidants. Vitamins A, C, E, many of the B vitamins, and minerals like magnesium, selenium and zinc are all especially helpful in lowering inflammation and uveitis risk.
When to See a Doctor
See a doctor immediately if you have any symptoms of uveitis, even if you think they are not serious. This disease can lead to permanent vision loss of it is not treated. Early detection is critical to ensuring the best outcomes with this dangerous condition.
References
-
Uveitis: Symptoms and Causes. (June 2020). Mayo Clinic.
-
Uveitis. (November 2021). National Eye Institute.
-
What is Uveitis? (November 2021). American Academy of Ophthalmology.
-
Exercise May Stave Off Eye Disease, Study Finds. (October 2020). American Academy of Ophthalmology.
-
Uveitis. (2022). Icahn School of Medicine at Mount Sinai.
-
Cigarette smoking as a risk factor for uveitis. (March 2010). Ophthalmology.
-
Treatment: Uveitis. (January 2020). National Health Service.
-
Uveitis: Diagnosis. (June 2020). Mayo Clinic.
-
Uveitis. (February 2021). Cleveland Clinic.
-
Epidemiology of uveitis in a US population-based study. (April 2018). Journal of Ophthalmic Inflammation and Infection.
-
Eyes – uveitis. (September 2020). Better Health Channel.
-
Uveitis. (January 2020). National Health Service.
Last Updated March 23, 2022
Note: This page should not serve as a substitute for professional medical advice from a doctor or specialist. Please review our about page for more information.