Periorbital Cellulitis
Periorbital cellulitis is an infection of eyelid tissues and of skin around the eye. Although people of all ages can get this condition, it is more common in children than adults.
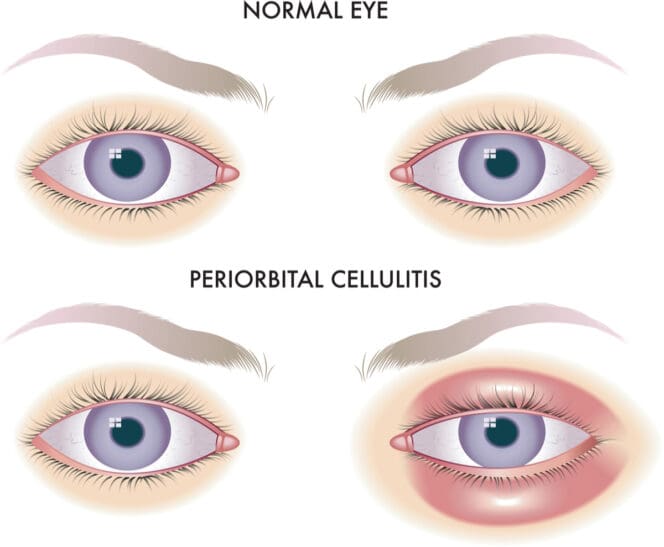
Symptoms usually occur to one eye only, and the most common symptom is inflammation of the eyelid or surrounding skin as well as changing color.
Most cases resolve within a week of taking antibiotics. In rare cases, the infection can cause complications, particularly when untreated.
This condition does not affect vision or cause pain in the eye.
Introduction
Periorbital cellulitis, also referred to as preseptal cellulitis, is an infection in the tissues around on eyelids and on skin around the eye. Although people of all ages can get this condition, it is more common in children than adults.
The infection occurs when germs get into the skin through a scratch or cut or get to the area through another infection such as a sinus infection.
Germs infect the area in front of the orbital septum, which separates the frontal structures of the eyelid from the back portion, orbit. They cause redness, tenderness and swelling of the eyelid and the skin surrounding your eyes.
Most cases resolve within a week of taking antibiotics. In rare cases, the infection can cause complications, particularly when untreated.
Eye specialists recommend having any eye-related irritants and diagnosed and treated promptly to prevent complications that can include permanent vision problems and even blindness in extreme cases. It is not contagious.
Periorbital cellulitis is not to be confused with orbital cellulitis, a rarer and more serious infection of the fat and muscles around the eye behind the orbital septum. Orbital cellulitis can cause deeper infections and lasting problems.
Causes of Periorbital Cellulitis
Periorbital cellulitis is caused by germs that enter the skin through a cut, scratch, insect bite, puncture wound, sore, dog bite or an infected bump such as a stye. Germs can also originate from a cold or sinus infection.
Children who frequently fight colds or sinus infections are more likely to develop periorbital cellulitis. In fact, according to the American Academy of Ophthalmology, cellulitis is more common during the winter because it is the time of year people tend to develop sinus infections.
A bacterial infection can also cause periorbital cellulitis. Some of the common bacteria that cause it include:
- Staphylococcus – commonly found on the skin and in the nose
- Haemophilus influenzae
- Streptococcus – often causes strep throat
- Other infectious organisms such as viruses and fungi
Symptoms of Periorbital Cellulitis
Children and adults experience the same symptoms, although children might have more dramatic and severe symptoms. Symptoms typically occur around one eye only, either on the eyelid or around the eye.
The most common symptom is inflammation of the eyelid or the surrounding skin, as well as changing color. The British Association of Dermatologists notes that for people with white skin, the affected area might turn red or pink while people with brown or black skin may appear purple. There may also be a slight darkening of the existing skin color in some cases.
Other typical symptoms include:
- Pain and tenderness around the eye
- Redness in the white part of the eye
- Swelling of the white part of the eye
- Irritability around the affected eye
- Low-grade fever
This condition does not affect vision or cause pain in the eye.
Diagnosis of Periorbital Cellulitis
To diagnose periorbital cellulitis, doctors:
- Take a medical history and ask questions such as whether you had any recent injuries or infections, scratches, bug bites, or breaks in the skin.
- Conduct a visual examination, checking whether your eyes move naturally and respond appropriately to light.
- Conduct an eye exam to check the symptoms, look for any injury, or see if there is another infected bump that could have led to the condition, such as a stye.
Your doctor may also:
- Check your eye pressure to make sure it’s normal
- Take a blood sample to identify the bacteria involved or other infection-related changes in the blood.
- Take eye secretions to test and identify the bacteria involved
Your doctor may also order the following imaging tests to see how far the infection has spread and to confirm that it is indeed periorbital cellulitis and not orbital cellulitis.
- CT scan (computerized tomography)
- X-rays
- MRI scan
Treatment Options for Periorbital Cellulitis
Early intervention can help improve the outlook for people with periorbital cellulitis. As such, periorbital cellulitis is typically not a major cause for concern. However, without treatment or if treatment is delayed the condition can progress and cause serious complications.
Doctors have several treatment options. Which treatment depends on the person’s age and the progression of the infection.
For patients over the age of 1, doctors will prescribe oral antibiotics. Infants younger than 1 or with a severe infection may need intravenous (IV) antibiotics.
Doctors prefer several antibiotics to treat periorbital cellulitis. Among them are:
- Amoxicillin
- Trimethoprim
- Cefuroxime
- Doxycycline
- Piperacillin
- Ceftriaxone
The infection typically responds well to medication, with visible signs of improvement within one or two days and resolves quickly. Most people see full results within seven days.
In rare circumstances when symptoms don’t improve, doctors may need to drain any abscesses.
In extreme cases with no treatment is administered, the infection might spread into the eye socket, resulting in orbital cellulitis and its related complications.
Complications Associated with Periorbital Cellulitis
Absent treatment, periodontal cellulitis can lead to severe complications such as:
Outlook for People with Periorbital Cellulitis
Periorbital cellulitis is typically not a major cause for concern when detected early. While some minor eye infections, such as pinkeye or stye, will go away on their own, periorbital cellulitis requires treatment with antibiotics.
When to Call a Doctor
Contact your doctor immediately if:
- Your eye starts becoming red or swollen
- Symptoms get worse after treatment
- A fever develops along with eye symptoms
- It becomes difficult or painful to move the eye
- Your eye looks like it is sticking out (bulging)
- You notice vision changes
Frequently Asked Questions about Periorbital Cellulitis
How serious is periorbital cellulitis?
Although periorbital cellulitis, is largely not a major concern, with inadequate treatment, this condition can lead to complications such as subperiosteal abscess, orbital cellulitis and cavernous sinus thrombosis. Treatment helps stop the spread of infection to other areas of the eye.
Is periorbital cellulitis an emergency?
Although periorbital swelling is common and largely not a major concern, it can quickly progress into a serious condition if left untreated. If you experience the symptoms of periorbital cellulitis coupled with fever, pain with eye movement, bulging eye or changes in vision, contact your doctor right away or present yourself to the nearest hospital immediately. And even in the case that you only experience the base symptoms, you should make sure you see your doctor as soon as possible.
How Do I know if I have periorbital cellulitis?
The most common signs that might indicate you might have periorbital cellulitis are:
- Tenderness and swelling around the eye
- Reddish or slightly purple bump close to the eye
- Redness in the white part of the eye
- Swelling of the white part of the eye
- Irritability around the affected eye
- Low-grade fever
However, these symptoms are not a fool-proof test on whether you have periorbital cellulitis. Only your doctor can tell you definitively whether you have it, and only after examining your eye, analyzing your blood and eye secretions and reviewing your medical history.
If you notice any of the symptoms listed above, contact your doctor as soon as possible.
References
-
Periorbital Cellulitis. (July 2021). StatPearls.
-
Periorbital and Orbital Cellulitis. (January 2020). Journal of the American Medical Association.
-
Orbital cellulitis. (October 2020). Icahn School of Medicine at Mount Sinai.
-
What Is Cellulitis? (November 2021). American Academy of Ophthalmology.
-
Describing Erythema in Skin of Colour. (March 2015) British Association of Dermatologists.
-
Paediatric periorbital cellulitis: A 10-year retrospective case series review. (September 2020). Wiley Online Library.
-
Subperiosteal abscess of the orbit. (May 1983). Archives of Ophthalmology.
-
Orbital Cellulitis and Abscess. (September 2010). The Western Journal of Ophthalmology.
-
Cavernous sinus thrombosis. (August 2021). National Health Services.
Last Updated March 1, 2022
Note: This page should not serve as a substitute for professional medical advice from a doctor or specialist. Please review our about page for more information.