Home /
Retinopathy: Symptoms, Treatment, and Causes
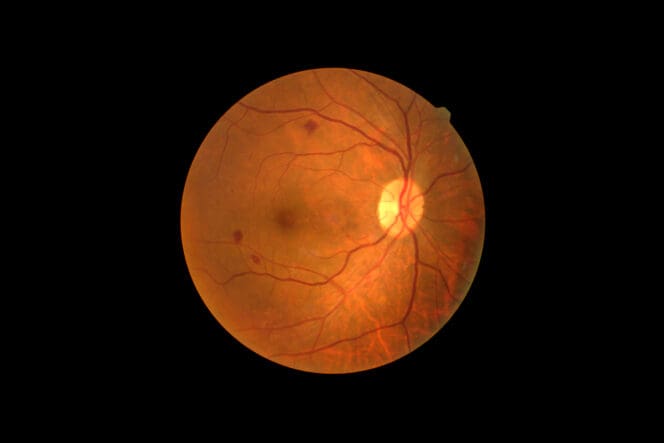
Retinopathy refers to any damage to the retina, a light-sensitive tissue layer at the back of the eye. The retina communicates with the brain to help you recognize images and any information you see or read.
When your retina is not working properly, your vision can decline. Several conditions, including diabetes and high blood pressure, can cause retinopathy.
Managing the cause of your retinopathy is the most effective way to prevent vision loss.
Types of Retinopathy
There are several types of retinopathy, but the three most primary types are diabetic retinopathy, hypertensive retinopathy and retinopathy of prematurity.
- Diabetic retinopathy: Diabetic retinopathy means damage to weak blood vessels in the retina as a result of diabetes. Uncontrolled levels of sugar in your blood can cause this eye condition, increasing your risk for vision loss.
- Hypertensive retinopathy: With hypertensive retinopathy, high blood pressure causes retinal damage. The condition affects veins and arteries that supply blood to the retina. Left untreated, severe hypertension may cause irreversible damage to parts of the eye like the optic nerve. Blindness can eventually occur.
- Retinopathy of prematurity (ROP): Retinopathy of prematurity occurs in premature babies, especially small infants. This eye disorder affects retinal blood vessels and can cause childhood blindness.
Signs
Retinopathy doesn’t usually have early symptoms, but eye exams can detect retinal damage. Regardless of the cause, advanced cases can have vision problems such as:
- Vision loss
- Dim vision
- Double vision
- Fluctuating vision
- Eye floaters
- Blind spots
- White pupil or abnormal eye movements in retinopathy of prematurity
Physical signs of retinopathy that eye exams can help detect include:
- Swollen optic nerve
- Leaking blood vessels (bleeding in the eye)
- Narrow eye blood vessels
- Damaged/blocked eye blood vessels
- Edema, which is fluid buildup in the center part of the retina called macula
- Thick, twisted blood vessels of the retina
Causes
Retinopathy has various potential causes, and cause usually are a clue to the type of retinopathy somebody has. These include:
Diabetic retinopathy: When there’s too much sugar in your blood due to diabetes, blockage of the small vessels that supply the retina can occur. New but weaker blood vessels grow to keep blood and nutrition flowing into the retina. These weak vessels can leak blood, damaging the retina.
Hypertensive retinopathy: In one study, 83.6 percent of patients with high blood pressure had hypertensive retinopathy. This condition exerts excessive pressure on retinal blood vessels, damaging them.
Retinopathy of prematurity: Retinopathy of prematurity occurs in babies with underdeveloped retinal blood vessels. The eye compensates for this by growing abnormal, fragile vessels that may eventually break down and leak blood.
Risk Factors
Factors that may elevate your risk for retinopathy include:
- Diabetes
- Uncontrolled blood sugar levels
- Uncontrolled high blood pressure
- Cholesterol
- Genetics (family history)
- Smoking
- Arteriosclerosis (thick and stiff retinal arteries restrict blood flow in the eye)
- Smoking
Predisposing factors for ROP in babies may include:
- Poor infant health
- Breathing problems
- Low levels of healthy blood cells (anemia)
- Respiratory problems
- Premature birth (babies born before the 31st week of pregnancy (gestation)
- Premature infants weighing about two and half pounds (1250 g) or less
- Blood transfusions
Complications
All types of retinopathy expose an individual to severe vision and overall health issues. Potential complications include:
- Blindness
- Macular edema (accumulation of fluid in the middle portion of the retina)
- Optic nerve damage, which can cause glaucoma and blindness
- Vitreous hemorrhage (bleeding in the eye), which can reduce or block your eyesight
- Blockage of retinal blood vessels
- Age-related macular degeneration, which can cause blurred central vision
- Retinal detachment (abnormal weak blood vessels leak, scarring and pulling the retina out of its natural position)
- Severe hypertensive retinopathy can cause permanent vision loss
- Patients with severe hypertensive retinopathy are at a high risk for stroke, heart problems and kidney complications
- Babies with ROP may develop eye disorders like refractive errors, crossed eyes and lazy eyes when older
Diagnosis
Your ophthalmologist may run several tests to diagnose the level of retinal damage in your eye. Eye exams for retinopathy include a fluorescein angioplasty and a ophthalmoscopy.
Fluorescein angiography
This test helps to detect blood flow problems, including leaks and blockages in retinal blood vessels. Your doctor will first dilate your pupils to get a better view.
Next, they’ll inject a dye into a vein in your arm. Using a special camera-like instrument, they’ll capture images that show flow of the dye (and blood) through your retinal vessels.
Ophthalmoscopy
Ophthalmoscopy or fundoscopic exam lets your ophthalmologist observe the back part of your eye or fundus.
This section includes the retina and optic disc. Examining it can reveal any issues affecting blood vessels that nourish the retina.
You may have retinopathy if your ophthalmoscopy exam detects any of the following:
- Swollen, narrow, or blocked retinal blood vessels
- Swollen optic nerve
- Macular edema
- Blood leaks
Your primary care physician may be involved if blood sugar and hypertension tests are required.
Retinopathy Treatment
The type and severity of your eye condition determines your most effective treatment. Mild retinopathy usually resolves without intervention, regardless of the cause.
Treating Hypertensive Retinopathy
High blood pressure rarely causes significant vision problems. Nonetheless, it should be managed to protect your eyes and overall health.
The best line of defense against hypertensive retinopathy is blood pressure control with regular checkup. Your retina can recover after lowering your BP.
In severe cases, this condition can cause permanent eye damage even after medically regulating the patient’s BP.
Treating Diabetic Retinopathy
Treatment options for severe diabetic retinopathy include:
- Vascular endothelial growth factor (VEGF) inhibitors. Anti-VEGF medication halts the growth of abnormal blood vessels in your eye. Using these drugs with diabetes minimizes the risk of fluid leakage and buildup and retinal scarring and detachment.
- Laser therapy. Laser treatment stops the blood leaks in your eye, halting detrimental fluid buildup. It is a form of targeted therapy that destroys the leak-causing abnormal blood vessels.
- Surgery. Your eye surgeon may use vitrectomy, a slightly invasive eye surgery, to halt retinal damage. They’ll make a small cut into the center area of your eye to remove accumulated fluid. During this procedure, the doctor can also cut out the scarring tissue responsible for retinal detachment.
Treating Retinopathy of Prematurity
Mild cases of ROP require no treatment as they are usually not vision-threatening. Severe cases may warrant invasive intervention, such as eye injections, surgery, and laser therapy.
Scleral buckle is another surgical option for infants with ROP to prevent retinal detachment. With this procedure, an ophthalmologist stitches an artificial band around the eye, tightening it.
Prevention
To avoid retinopathy, you must control any existing condition that might cause it. A healthy lifestyle reinforces your vision protection if you’re diabetic or hypertensive.
Preventative measures include:
- Regular physical exercise
- Eating healthy
- Cholesterol control (minimizes risk for arteriosclerosis and narrowing of blood vessels supplying the retina)
- Diabetes/blood sugar control with insulin therapy as directed by your doctor
- Avoiding tobacco
- Blood pressure control, including with medication
- Regular eye exams
- Ongoing hypertension monitoring
- Regular hemoglobin A1C tests every two or three months to estimate your average blood sugar level
References
-
Diabetic Retinopathy. (June 2021). Mayo Clinic.
-
High Blood Pressure and Eye Disease. (February 2022). MedlinePlus.
-
Retinopathy of Prematurity. (July 2019). National Eye Institute. Date Fetched: January 28, 2022
-
Hypertensive Retinopathy. StatPearls.
Last Updated February 28, 2022
Note: This page should not serve as a substitute for professional medical advice from a doctor or specialist. Please review our about page for more information.