Home /
Diabetic Retinopathy: Symptoms, Treatment, Prevention
Diabetic retinopathy is when diabetes (too much blood glucose) causes retinal damage, potentially affecting vision.
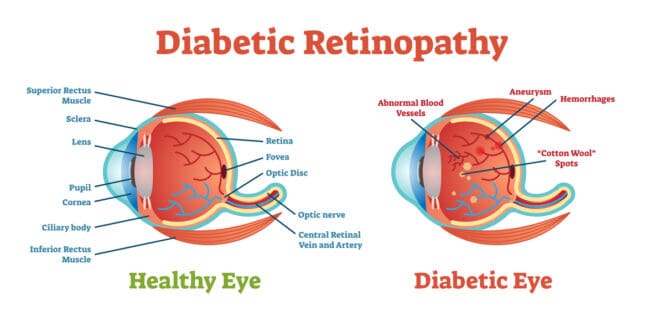
The retina is a tissue layer at the back of the eye that captures and sends information to the brain, enabling you to see. Damage can occur when retinal blood vessels swell, leak or clog.
When your retina malfunctions due to diabetes, you may experience a degree of vision loss. Early treatment and diabetes control can halt or even reverse retinopathy, preventing complete blindness.
Stages of Diabetic Retinopathy
Diabetic retinopathy develops through two main stages. These are:
- Non-proliferative diabetic retinopathy (NPDR)
- Proliferative diabetic retinopathy (PDR)
Non-Proliferative Diabetic Retinopathy (NPDR)
Two main developments occur at this stage: blood vessel leaks and blockages. Although vision loss can occur, this is the best time to start monitoring your condition.
Blood can accumulate in the macula in the retina (macular edema), causing swelling and slight vision problems. The tiny retinal vessels can also close off as damage continues.
When this happens, supply of oxygen and nutrients to the macula declines as does the sharpness of your eyesight.
Proliferative Diabetic Retinopathy (PDR)
PDR is most severe vision-threatening phase of this eye condition. It gets its name from the proliferation of abnormal retinal blood vessels.
The anomalous growths aren’t as strong as normal blood vessels in the retina. They can eventually leak blood into vitreous, the gel-like fluid in the middle area of your eye.
Vitreous is clear in a healthy eye, but blood leaks can taint it, obstructing vision. Depending on severity of the bleeding, you may lose part or all of your eyesight.
Symptoms
Although retinopathy is always a possibility when you’re diabetic, it often begins without any outward signs. You may experience symptoms such as below if your condition keeps getting worse:
- Eye floaters
- Blind spots in your vision
- Declining vision
- Hazy vision
- Poor night vision
Complications
Left untreated, diabetic retinopathy can cause significant damage to different parts of the eye as it progresses. Any of the affected tissues may eventually compromise your vision. In severe cases, it can lead to complete blindness.
Watch out for complications such as:
- Vision loss from vitreous bleeding
- Blindness if the retina detaches from the back of the eye
- Vision-threatening glaucoma due to optic nerve damage
Causes
When you have diabetes, your blood sugar level is above healthy levels. Diabetic retinopathy can develop when small vessels that supply blood to the retina close off.
Another possibility is the swelling of your retina once blood vessels in it start leaking. Fluid can build up in the macula because of the leaks.
Retinal damage occurs during the early stages of diabetic retinopathy.
Diagnosis
Some patients may require multiple diabetic retinopathy tests to get a conclusive diagnosis. Options include:
Dilated eye exam: Dilating drops will widen your pupils, giving your eye doctor a clear view of the back of your eye. Using a magnifying lens, the specialist can examine tissues like the retina, macula, and optic nerve.
Optical coherence tomography (OCT): Your doctor may run OCT scans of the retina to detect and measure any retinal swelling.
Fluorescein angiography: Fluorescein angiography can help your ophthalmologist spot problems impacting retinal blood flow. The test begins with a dye shot into a vein in your body.
A specialty camera takes pictures of your retina as the dye circulates through the retinal blood vessels. The captured photos can show any blood vessel abnormalities, leaks, or constrictions at the back of the eye.
Risk Factors
Uncontrolled diabetes is the primary predisposing factor for diabetic retinopathy. Your lifestyle and other elements of your overall body health can impact your risk for the eye disorder.
Common risk factors include:
- Hypertension (high blood pressure)
- Uncontrolled blood sugar level
- Pregnancy
- High cholesterol levels in your blood
- Tobacco consumption
Treatment
It’s important that you cooperate closely with your primary care physician and eye doctor to manage your condition. Treatment options for diabetic retinopathy include:
Diabetes and hypertension management
Keeping blood sugar levels down can halt disease progression or reverse some vision damage. Blood pressure control keeps your eye blood vessels healthy, helping protect your vision.
Eye injections
Vascular endothelial growth factor (VEGF) inhibitors are eye injections for macular swelling. FDA-approved options include ranibizumab (Lucentis) and aflibercept (Eylea).
These anti-VEGF injections can control fluid buildup in the macula to halt or even reverse vision degradation.
Laser therapy
Laser surgery can treat retinopathy in several ways. It can close off leaky blood vessels or destroy abnormal fragile vessels causing vitreous bleeding.
Vitrectomy
During vitrectomy, your eye surgeon or ophthalmologist cuts the vitreous gel out of your eye. The surgical procedure can also remove any blood that’s accumulated in the back of the eye.
Prevention
Eye care, tests and comprehensive and disease-specific exams are always critical for optimizing your vision and overall health. Once you’re diagnosed with diabetes, these become high-urgency preventive measures.
Here are some tips to protect your vision health if you’re diabetic:
- Get comprehensive eye exams and tests regularly, such as pupil dilation, visual field, and eye pressure tests.
- Begin your retinopathy treatment as soon as you test positive for the condition.
- Burn the extra calories to maximize fitness with moderate physical exercise every day.
- Watch your blood sugar level (with a proper diet and insulin or any diabetes drug as directed by your doctor).
- Watch your blood pressure. (Research shows that hypertension management in patients with diabetic retinopathy can reduce the risk of vision loss.)
- Let your eye doctor know if you experience any vision changes.
Eat healthy
Your nutritionist can help you create a healthy diet plan to control your blood sugar. The best diets for people with hypertension or diabetes include:
- Low-fat dairy products
- Whole grains
- Nuts
- Low cholesterol
- Low saturated fat
- Fiber-rich
- Protein-rich
- Calcium-rich
- Magnesium-rich
Nutritional supplements
Supplements can be an option for people not getting enough nutrients from their daily diet. Consult your doctor and nutritionist about benefits and side effects before consuming any supplementary nutrition or herbal products.
FAQs
What are the stages of diabetic retinopathy?
Non-proliferative diabetic retinopathy (NPDR) is the first stage. Retinal damage is moderate and there are no abnormal blood vessels supplying the retina.
The last stage is proliferative diabetic retinopathy (PDR). Severe retinal damage can occur here, with loss of central and side vision.
What causes diabetic retinopathy?
Diabetic retinopathy can develop when you have uncontrolled, high blood sugar levels. The condition may damage the retina due to blood vessel blockages and leaks at the back of the eye.
Can diabetic retinopathy be corrected?
Early diagnosis and treatment improve your chances of recovery from the effects of retinopathy on your eyesight. Eye injections and surgery may help prevent further vision loss or perhaps reverse it in some cases.
References
-
Diabetic Retinopathy: Causes, Symptoms, Treatment. (September 2021). American Academy of Ophthalmology.
-
Diabetic Retinopathy. (June 2021). Mayo Clinic.
-
Hypertension and Diabetic Retinopathy—What’s the Story? (September 1999). British Journal of Ophthalmology.
-
DASH Eating Plan: an Eating Pattern for Diabetes Management. (May 2017). American Diabetes Association.
Last Updated February 28, 2022
Note: This page should not serve as a substitute for professional medical advice from a doctor or specialist. Please review our about page for more information.